What’s Trending?
COVID-19 Vaccine Information
Flu Season Information
Flu Season FAQ's
Teens Nutritional Risk
Beat the Summer Heat
Staying Bug-Free
Bronchiolitis
Monkeypox
COVID-19 Vaccine Information

The vaccination process is about to get a little easier next week. Retail pharmacies will now start to get direct federal shipments of mRNA vaccines (Both Pfizer and Moderna), instead of having to go through a state distribution process weekly. This has been verified in my conversations with local pharmacists.
Most people have asked when are retail pharmacies like HEB going to receive and administer the vaccine? When will they add more appointment slots to their scheduler? The reality is that each state determined which entities received an allocation every week. Now, some pharmacies (NOT ALL) will begin to receive direct federal allocations. The new program (The Federal Retail Pharmacy Program), which will begin on February 11, will start at about 6,500 retail pharmacies nationwide. They will receive a total of 1 million doses. The program will eventually expand to other pharmacies. Yes. H-E-B, Walgreens, Walmart, CVS are included in that list of pharmacies.
In addition, the government is increasing the weekly allocation of vaccines going to states, tribes and territories by an additional 5%, bringing the weekly total of vaccines purchased per week to a minimum of 10.5 million.
The CDC is working with states to select pharmacy sites, which will take into account "their ability to reach some of the populations most at risk for severe illness from Covid-19, including socially vulnerable communities.”
So, be on the lookout for appointment slots on the HEB scheduler and other retail pharmacy schedulers. They could be popping up very soon.
Here is a list of the web addresses where you could make an appointment for vaccination at each perspective retail pharmacy.
H‑E‑B: https://vaccine.heb.com/scheduler
Walgreens: https://www.walgreens.com/findcare/vaccination/covid-19
CVS: https://www.cvs.com/immunizations/covid-19-vaccine?icid=cvs-home-hero1-banner-1-coronavirus-vaccine
(Appointments will become available for booking as early as Feb. 9)
Walmart: https://www.walmart.com/cp/1228302
CDC: vaccines.gov
Reference:
https://www.whitehouse.gov/briefing-room/statements-releases/2021/02/02/fact-sheet-president-biden-announces-increased-vaccine-supply-initial-launch-of-the-federal-retail-pharmacy-program-and-expansion-of-fema-reimbursement-to-states/
Flu Season Information

Seasonal flu activity has been intense this season. As of February 16, 2018 most of the United States continues to experience intense and widespread flu activity, with record-breaking levels of influenza-like-illness and hospitalization rates recorded. While H3N2 viruses are still most common, there is an increasing number of influenza B viruses being detected. It’s not uncommon for second waves of B virus activity to occur during a flu season. It’s likely that flu activity will continue for several more weeks.
Here are some important things to know right now to protect yourself and your loved ones from flu:
1. What are the symptoms of flu?
Flu viruses can cause mild to severe illness, and at times can lead to death. The flu is different from a cold. The flu usually comes on suddenly. People who have the flu often feel some or all of these symptoms:
• Fever* or feeling feverish/chills
• Cough
• Sore throat
• Runny or stuffy nose
• Muscle or body aches
• Headaches
• Fatigue (tiredness)
• Some people may have vomiting and diarrhea, though this is more common in children than adults
* It’s important to note that not everyone with flu will have a fever.
2. What do I do if I get sick?
Most people with the flu have mild illness and do not need medical care or antiviral drugs. If you get flu symptoms, in most cases you should stay home and avoid contact with other people, except to get medical care.
CDC recommends that antiviral drugs be used early to treat people who are very sick with the flu (for example, people who are in the hospital) and people who are sick with the flu and are at high risk of serious flu complications, either because of their age or because they have a high risk medical condition.
3. Is it too late to get a flu shot?
No! As long as flu viruses are still circulating, it is not too late to get a flu shot. Flu vaccination is the best way to prevent flu illness and serious flu complications, including those that can result in hospitalization. Unfortunately, flu vaccines don’t work as well against H3N2 viruses, which means that some people who got vaccinated will still get sick; however, there are some data to suggest that flu vaccination may make illness milder. Flu vaccines usually work better against H1N1 viruses, which is another good reason to get vaccinated, since H1N1 is circulating too.
4. Why should I get a flu shot?
In addition to protecting yourself, getting vaccinated also protects people around you, including people who are more vulnerable to serious flu illness, like babies and young children, older people, pregnant women and people with certain chronic health conditions.
5. Does the flu shot work?
Vaccine effectiveness data for this season are not available yet, but we know that flu vaccines do not work as well against H3N2 viruses, which are predominant so far this season.
6. What else can I do to protect myself from flu?
Definitely try to avoid close contact with sick people. If you do get sick, limit contact with others as much as possible to keep from infecting them. Stay home for at least 24 hours after your fever is gone without the use of fever-reducing drugs (unless you need medical care or other necessities).
Other tips for stopping the spread of germs:
• Make sure you cover your nose and mouth with a tissue when you cough or sneeze. Throw the tissue in the trash after you use it.
• Wash your hands often with soap and water.
• Avoid touching your eyes, nose, and mouth. Germs spread this way!
• Clean and disinfect surfaces and objects that may be contaminated with germs like the flu.
Frequently Asked Flu Questions About the Influenza Season

When should I get vaccinated?
It’s best to get vaccinated before flu begins spreading in your community; however, CDC continues to recommend flu vaccination as long as flu viruses are circulating since vaccination later can still be beneficial during most seasons. Given influenza activity levels as of February 3, 2018 and an increasing proportion of influenza B and H1N1 viruses being detected, CDC continues to recommend flu vaccination this season. It takes about two weeks after vaccination for antibodies to develop in the body that protect against flu.
Children who need two doses of vaccine to be protected should start the vaccination process sooner, because the two doses must be given at least four weeks apart.
Can I get a flu vaccine if I am allergic to eggs?
The recommendations for people with egg allergies are the same as last season.
• People who have experienced only hives after exposure to egg can get any licensed flu vaccine that is otherwise appropriate for their age and health.
• People who have symptoms other than hives after exposure to eggs, such as angioedema, respiratory distress, lightheadedness, or recurrent emesis; or who have needed epinephrine or another emergency medical intervention, also can get any licensed flu vaccine that is otherwise appropriate for their age and health, but the vaccine should be given in a medical setting and be supervised by a health care provider who is able to recognize and manage severe allergic conditions. (Settings include hospitals, clinics, health departments, and physician offices). People with egg allergies no longer have to wait 30 minutes after receiving their vaccine.
Will new flu viruses circulate this season?
Almost all of the flu viruses examined this season are still similar to the cell-grown vaccine reference viruses which means we are not seeing significant antigenic drift in the circulating viruses based on CDC laboratory testing.
Will the United States have a flu epidemic?
The United States experiences epidemics of seasonal flu each year. This time of year, is called “flu season.” In the United States, flu viruses are most common during the fall and winter months. Influenza activity often begins to increase in October and November. Most of the time flu activity peaks between December and February and can last as late as May. CDC monitors certain key flu indicators (for example, outpatient visits of influenza-like illness (ILI), the results of laboratory testing and reports of flu hospitalizations and deaths). When these indicators rise and remain elevated for a number of consecutive weeks, “flu season” is said to have begun. Usually ILI increases first, followed by an increase in flu-associated hospitalizations, which is then followed by increases in flu-associated deaths. This season, ILI went above baseline in late November and remained elevated through February 3, 2018.
How many people are hospitalized from flu every year?
CDC estimates the total number of flu-associated hospitalizations in the United States. CDC monitors rates of lab confirmed flu-associated hospitalizations in about 9% of the U.S. population, and it collects information only on hospitalizations that had a positive flu test. We know that not everyone with an influenza related hospitalization will be captured in this system because not everyone gets a flu test and those that do may not have a positive result if many days have passed since they first became sick. That is why CDC also uses mathematical modeling to fill in the picture of the disease burden. Since 2010, CDC estimates that flu has resulted in between 140,000 and 710,000 hospitalizations each year.
What should I do to protect myself from flu this season?
CDC recommends a yearly flu vaccine for everyone 6 months of age and older, even when reduced vaccine effectiveness against one or more flu viruses is expected or observed.
In addition to getting a seasonal flu vaccine, you can take everyday preventive actions like staying away from sick people and washing your hands to reduce the spread of germs. If you are sick with flu, stay home from work or school to prevent spreading flu to others. In addition, there are prescription medications called antiviral drugs that can be used to treat influenza illness.
What should I do to protect my loved ones from flu this season?
Elevated levels of flu activity are expected to continue for several weeks so there is still time to, encourage your loved ones to get vaccinated. Vaccination is especially important for people at high risk for developing flu complications, and their close contacts. Also, if you have a loved one who is at high risk of flu complications and they develop flu symptoms, encourage them to get a medical evaluation for possible treatment with flu antiviral drugs. These drugs work best if given within 48 hours of when symptoms start. CDC recommends that people who are at high risk for serious flu complications and who get flu symptoms during flu season be treated with flu antiviral drugs as quickly as possible without waiting for confirmatory testing. People who are not at high risk for serious flu complications may also be treated with flu antiviral drugs, especially if treatment can begin within 48 hours.
Do some children require two doses of flu vaccine?
Yes. Some children 6 months through 8 years of age will require two doses of flu vaccine for adequate protection from flu. Children in this age group who are getting vaccinated for the first time will need two doses of flu vaccine, spaced at least 28 days apart. Children who have only received one dose in their lifetime also need two doses. Your child’s doctor or other health care professional can tell you if your child needs two doses of flu vaccine.
What can I do to protect children who are too young to get vaccinated?
Children younger than 6 months old are at high risk of serious flu complications, but are too young to get a flu vaccine. Because of this, safeguarding them from flu is especially important. If you live with or care for an infant younger than 6 months old, you should get a flu vaccine to help protect them from flu. Everyone else who is around the baby also should be vaccinated. Also, studies have shown that flu vaccination of the mother during pregnancy can protect the baby after birth from flu infection for several months.
In addition to getting vaccinated, you and your loved ones can take everyday preventive actions like staying away from sick people and washing your hands to reduce the spread of germs. If you are sick with flu, stay home from work or school to prevent spreading flu to others.
Will live attenuated intranasal influenza vaccine (LAIV) be available this season even though it is not recommended for use?
FluMist® Quadrivalent is still an FDA-licensed product. As such, there may be some supply of FluMist® Quadrivalent on the U.S. market during the 2017-2018 season. It is important for clinicians and the public to be aware that because of concerns about this vaccine’s effectiveness, CDC recommends that this vaccine not be used during the 2017-2018 influenza season.
CDC: Teens Missing Nutritional Mark

Teenagers are often found facing a screen—whether it’s a phone, television, computer, or video game. Although digital media has some benefits, the extent to which children and adolescents rely on media is highlighted in a new report that studies common healthy—and unhealthy—behaviors in young persons today.
Data on digital media use and other health activity trends, such as nutritional choices and physical activity, among children and teenagers were unveiled earlier this year in the newest Youth Risk Behavior Survey (YRBS)1 from the Centers for Disease Control and Prevention (CDC). The survey identifies health-related behaviors and trends across 6 categories every 2 years to compile a national report assessing adolescent health risks.
The report monitors 6 categories of health-related behaviors among adolescents and young adults: behaviors that contribute to unintentional injuries and violence; tobacco use; alcohol and other drug use; sexual behaviors related to unintended pregnancy and sexually transmitted infections (STIs), including human immunodeficiency virus (HIV) infection; unhealthy dietary behaviors; and physical inactivity.
The entire report summarizes a total of 121 health-related behaviors of students across 39 states. Contemporary Pediatrics previously covered the report’s findings on alcohol and drug use, sexual behaviors, and other high-risk behaviors.2 This report will focus on dietary behaviors and physical activity trends.
According to the CDC, 43% of the students studied in the report played video or computer games, or used a computer for 3 or more hours each day—above the previously estimated 2 hours per day. The report points out that this usage increased from 22.1% to the current 43% between 2003 and 2017. This computer time happens on school days, but doesn’t necessarily involve the completion of school work, according to the report, and 15.4% of the teenagers studied were sedentary for at least an hour in the prior week that they were polled. The report adds that 14.8% of the teenagers polled were obese and 15.6% were overweight.
Adolescents also reported high rates of television use, with 20.7% watching 3 or more hours of television daily—although this rate was a decline from 42.8% in 1999.
The CDC reveals in a statement about the report findings that whereas physical activity is one of the most proactive things individuals can do for their health, children and teenagers are falling short in this category.
“American youth do not get the recommended amount of physical activity nor do they eat the recommended amounts of fruits and vegetables each day,” according to the CDC. “Regular physical activity can help children and adolescents improve cardiorespiratory fitness, build strong bones and muscles, control weight, reduce symptoms of anxiety and depression, and reduce the risk of developing health conditions such as heart disease, cancer, type 2 diabetes, high blood pressure, osteoporosis, and obesity,” the researchers write.
Some trends were promising, however, with nearly half—46.5%—of students reporting that they were active for at least an hour each day on 5 or more days during the week prior to the survey, and 26.1% of teenagers were active for at least an hour every day of the week. Additionally, 51.1% did strength or toning exercises at least 3 days each week, according to the report.
Physical education (PE) classes in school offer some motivation as well, with 51.7% of students attending PE classes at least 1 day a week at school, and about a third of students attending PE classes daily. Participation on sporting teams also remains popular, with 54.3% of students playing on at least 1 sports team through school or another organization.
In addition to regular physical activity, the CDC also recommends that children and adolescents eat 1 to 2 cups of fresh fruit and 1 to 3 cups of fresh vegetables daily. The report found, however, that 5.6% of teenagers had not eaten fresh fruit or drunk 100% fruit juice in the week prior to the survey. Another 60.8% had fruit or fruit juice at least once per day; 31.3% had 2 or more servings of fruit or fruit juice daily; and 18.8% had 3 or more servings of fruit or fruit juice daily in the week before the survey.
Rates of vegetable consumption were similar, with 7.2% not eating any fresh vegetables in the week before the survey. About 60% of teenagers had at least 1 serving of vegetables per day; 26.6% had 2 or more servings per day; and 13.9% had 3 or more servings per day in the week before the survey.
Aside from fresh fruits and vegetables, the survey found that milk consumption was also low, with 26.7% of teenagers not consuming any milk in the week before the survey. About 31% consumed at least 1 glass of milk daily; 17.5% had at least 2 glasses per day; and 7.9% drank at least 3 glasses of milk daily. On the positive side, roughly a third—27.8%—did not consume soda or pop in the week before the survey; 18.7% drank soda at least once a day; 12.5% drank 2 or more servings per day; and 7.1% drank 3 or more servings per day.
Most students also avoided sports drinks, according to the report, with 47.7% of students avoiding all sports drinks in the week prior to the survey. Water appeared to be the favored drink, with 51.3% of teenagers drinking 3 or more glasses or bottles of water daily. Almost 67% drank at least 2 servings of water daily; 75.4% drank at least 1 serving; and just 3.8% of teenagers reported not drinking any plain water at all in the week prior to the survey.
In terms of eating habits, the survey found that 14.1% of adolescents skip breakfast daily, whereas 35.3% eat breakfast every day, according to the report.
Other health issues addressed in the survey were the prevalence of certain conditions, such as asthma. The report notes that 22.5% of students had been told by a clinician that they had asthma, an increase from 18.9% in 2003.
The report also reviewed dental care, revealing that 1.5% of teenagers had never seen a dentist whereas 75.7% had been to a dentist in the year prior to the survey. Tanning bed use also was reviewed, with indoor tanning decreasing from 15.6% in 2009 to just 5.6% in 2017, according to the report. Still, exposure is a concern, with 57.2% of teenagers reporting 1 or more sunburns in the prior year whether from outdoor sun exposure or indoor tanning use.
Sleep was another concern addressed in the report. The CDC found that 25.4% of students got 8 or more hours of sleep on school nights, with levels of sleep decreasing as teenagers progressed through their high school years.
Kathleen Ethier, PhD, director of the Division of Adolescent and School Health for the CDC, says that overall this year’s report shows that adolescents are generally making better decisions about their health and the risks they take, but there is also more work to be done. Pediatricians are in a unique position to offer guidance on healthy food and activity choices, she says, as well as to offer education and support for preventive care. These efforts should be in conjunction with school and community programs, as well as family support, she says.
“Connectedness is key to protecting health of adolescents—to family, to peers, and to important adults in their schools and other community organizations, including their healthcare providers,” Ethier says. “Students are more likely to thrive if they know they matter—that they have adults, teachers, and friends who care about their safety and success—and these protections last into adulthood.”
Source:
Contemporary Pediatrics
Sun Safety and Protection Tips

Spending time outdoors is a common activity on spring breaks or summer vacations, but remember to protect against the sun's rays. Everyone is at risk for sunburn. Children especially need to be protected from the sun's burning rays, since most sun damage occurs in childhood. Like other burns, sunburn will leave the skin red, warm, and painful. In severe cases, it may cause blistering, fever, chills, headache, and a general feeling of illness. The American Academy of Pediatrics offers tips to keep children safe in the sun.
Sun Safety and Protection under 6 Months
• Babies under 6 months of age should be kept out of direct sunlight. Move your baby to the shade under a tree, umbrella or stroller canopy. Dress babies in lightweight clothing that covers the arms and legs, and use brimmed hats that shade the neck to prevent sunburn.
• When adequate clothing and shade are not available, parents can apply a minimal amount of sunscreen with at least 15 SPF It is okay to apply a small amount of sunscreen on infants under 6 months if there is no way to avoid the sun SPF (sun protection factor) to small areas, such as the infant's face and the back of the hands. Remember it takes 30 minutes to be effective.
• If an infant gets sunburn, apply cool compresses to the affected area.
Sun Safety for Kids
• The first, and best, line of defense against harmful ultraviolet radiation (UVR) exposure is covering up. Stay in the shade whenever possible, and limit sun exposure during the peak intensity hours - between 10 a.m. and 4 p.m.
• Select clothes made of tightly woven fabrics. Cotton clothing is both cool and protective. Try to find a wide-brimmed hat that can shade the cheeks, chin, ears and back of the neck. Sunglasses with ultraviolet (UV) protection are also a good idea for protecting your child's eyes.
• Apply sunscreen with an SPF 15 or greater to areas of your child's skin that aren't covered by clothing. Before applying, test the sunscreen on your child's back for an allergic reaction. Apply carefully around the eyes, avoiding eyelids. If a rash develops, talk with your pediatrician.
• Be sure to apply enough sunscreen -- about one ounce per sitting for a young adult.
• Reapply sunscreen every two hours, or after swimming or sweating.
• If your child gets sunburn that results in blistering, pain or fever, contact your pediatrician.
Sun Safety for the Family
• The sun's rays are the strongest between 10 a.m. and 4 p.m. Try to keep out of the sun during those hours.
• The sun's damaging UV rays can bounce back from sand, water, snow or concrete; so be particularly careful of these areas.
• Wear commercially available sun-protective clothing, like swim shirts.
• Most of the sun's rays can come through the clouds on an overcast day; so use sun protection even on cloudy days.
• When choosing a sunscreen, look for the words "broad-spectrum" on the label - it means that the sunscreen will protect against both ultraviolet B (UVB) and ultraviolet A (UVA) rays. Choose a water-resistant sunscreen and reapply every two hours or after swimming, sweating or towel drying. You may want to select a sunscreen that does not contain the ingredient oxybenzone, a sunscreen chemical that may have hormonal properties.
• Zinc oxide, a very effective sunscreen, can be used as extra protection on the nose, cheeks, top of the ears and on the shoulders.
• Use a sun protection factor (SPF) of at least 15. The additional benefits of using sunscreen with SPF 50+ are limited.
• Rub sunscreen in well, making sure to cover all exposed areas, especially the face, nose, ears, feet and hands, and even the backs of the knees.
• Put on sunscreen 30 minutes before going outdoors - it needs time to work on the skin.
• Sunscreens should be used for sun protection and not as a reason to stay in the sun longer.
Protecting Children from Extreme Heat: Information for Parents
Extreme heat can cause children to become sick in several ways. Make sure to protect your child from the heat as much as possible, watch for symptoms, and call your pediatrician if you see any develop.
Prevent the Effects of Extreme Heat:
When weather conditions do not pose a safety or individual health risk, children can and should play outdoors. A heat index at or above 90°F, as identified by the National Weather Service, poses a significant health risk. However, there are several steps you can take to beat the heat and protect your child from heat-related illness:
• Find an air-conditioned space. If your home does not have air-conditioning, find a nearby building that does. Libraries can be a great place for a cool retreat from the heat. If you live in a place where the air-conditioning is unpredictable, plan in advance for a safe place for you and your family to go during times when the temperatures are high.
• Stay hydrated. Encourage your children to drink water regularly and have it readily available—even before they ask for it. On hot days, infants receiving breast milk in a bottle can be given additional breast milk in a bottle, but they should not be given water—especially in the first six months of life. Infants receiving formula can be given additional formula in a bottle.
• Dress lightly. Dress your children in clothing that is light-colored, lightweight, and limited to one layer of absorbent material that will maximize the evaporation of sweat. Kids have a lower capacity for sweating than adults.
• Plan for extra rest time. Heat can often make children (and their parents) feel tired.
• Cool off. When your child is feeling hot, give them a cool bath or water mist to cool down. Swimming is another great way to cool off while staying active.
• Prevent the effects of sun exposure. See Sun Safety: Information for Parents About Sunburn & Sunscreen.
• Ask about policies. Talk to your child's caregiver, camp, coach or child care provider about their policies for protecting your children throughout the day—especially during outdoor play or exercise.
Potential Health Effects of Extreme Heat:
Extreme heat can make children sick in many ways, including:
• Dehydration
• Heat exhaustion
• Heat cramps
• Heat stroke
When to Call Your Pediatrician:
Call your pediatrician immediately if your child develops any of the following symptoms. Your pediatrician can advise you on the next best course of action and whether an immediate evaluation is needed.
• Feeling faint
• Extreme tiredness (e.g., unusually sleepy, drowsy, or hard to arouse)
• Headache
• Fever
• Intense thirst
• Not urinating for many hours
• Nausea
• Vomiting
• Breathing faster or deeper than normal
• Skin numbness or tingling
• Muscle aches
• Muscle spasms
Source:
American Academy of Pediatrics
Choosing an Insect Repellent for Your Child

Mosquitoes, biting flies, and tick bites can make children miserable. While most children have only mild reactions to insect bites, some children can become very sick.
One way to protect your child from biting insects is to use insect repellents. However, it’s important that insect repellents are used safely and correctly.
Read on for more information from the American Academy of Pediatrics (AAP) about types of repellents, DEET, using repellents safely, and other ways to protect your child from insect bites.
Types of Repellents:
Insect repellents come in many forms, including aerosols, sprays, liquids, creams, and sticks. Some are made from chemicals and some have natural ingredients.
Insect repellents prevent bites from biting insects but not stinging insects. Biting insects include mosquitoes, ticks, fleas, chiggers, and biting flies. Stinging insects include bees, hornets, and wasps.
NOTE: The following types of products are NOT
effective repellents:
• Wristbands soaked in chemical repellents
• Garlic or vitamin B1 taken by mouth
• Ultrasonic devices that give off sound waves designed to keep insects away
• Bird or bat houses
• Backyard bug zappers (Insects may actually be attracted to your yard).
About DEET:
DEET is a chemical used in insect repellents. The amount of DEET in insect repellents varies from product to product, so it’s important to read the label of any product you use. The amount of DEET may range from less than 10% to more than 30%. DEET greater than 30% doesn’t offer any additional protection.
Studies show that products with higher amounts of DEET protect people longer. For example, products with amounts around 10% may repel pests for about 2 hours, while products with amounts of about 24% last an average of 5 hours. But studies also show that products with amounts of DEET greater than 30% don’t offer any extra protection.
The AAP recommends that repellents should contain no more than 30% DEET when used on children. Insect repellents also are not recommended for children younger than 2 months.
Tips for Using Repellents Safely
Dos:
• Read the label and follow all directions and precautions.
• Only apply insect repellents on the outside of your child’s clothing and on exposed skin. Note: Permethrin-containing products should not be applied to skin.
• Spray repellents in open areas to avoid breathing them in.
• Use just enough repellent to cover your child’s clothing and exposed skin. Using more doesn’t make the repellent more effective. Avoid reapplying unless needed.
• Help apply insect repellent on young children. Supervise older children when using these products.
• Wash your children’s skin with soap and water to remove any repellent when they return indoors, and wash their clothing before they wear it again.
Dont's:
• Never apply insect repellent to children younger than 2 months.
• Never spray insect repellent directly onto your child’s face. Instead, spray a little on your hands first and then rub it on your child’s face. Avoid the eyes and mouth.
• Do not spray insect repellent on cuts, wounds, or irritated skin.
• Do not use products that combine DEET with sunscreen. The DEET may make the sun protection factor (SPF) less effective. These products can overexpose your child to DEET because the sunscreen needs to be reapplied often.
Reactions to Insect Repellents:
If you suspect that your child is having a reaction, such as a rash, to an insect repellent, stop using the product and wash your child’s skin with soap and water. Then call Poison Help at 1-800-222-1222 or your child’s doctor for help. If you go to your child’s doctor’s office, take the repellent container with you.
Other Ways to Protect Your Child from Insect Bites:
While you can’t prevent all insect bites, you can reduce the number your child receives by following these guidelines:
• Tell your child to avoid areas that attract flying insects, such as garbage cans, stagnant pools of water, and flowerbeds or orchards.
• Dress your child in long pants, a lightweight long-sleeved shirt, socks, and closed shoes when you know your child will be exposed to insects. A broad-brimmed hat can help to keep insects away from the face. Mosquito netting may be used over baby carriers or strollers in areas where your baby may be exposed to insects.
• Avoid dressing your child in clothing with bright colors or flowery prints because they seem to attract insects.
• Don’t use scented soaps, perfumes, or hair sprays on your child because they may attract insects.
• Keep door and window screens in good repair.
• Check your child’s skin at the end of the day if you live in an area where ticks are present and your child has been playing outdoors.
• Remember that the most effective repellent for ticks is permethrin. It should not be applied to skin but on your child’s clothing.
Source:
American Academy of Pediatrics
ABOUT BRONCHIOLITIS

Bronchiolitis is a common illness of the respiratory tract . It's caused by an infection that affects the tiny airways, called the bronchioles, that lead to the lungs. As these airways become inflamed, they swell and fill with mucus, which can make breathing difficult.
Bronchiolitis:
- most often affects infants and young children because their noses and small airways can become blocked more easily than those of older kids or adults
- typically happens during the first 2 years of life, most commonly at about 3 to 6 months of age
- is more common in males, premature babies, children who have not been breastfed, and those who live in crowded conditions
Bronchiolitis is usually caused by a viral infection, most commonly respiratory syncytial virus (RSV) . RSV infections are responsible for more than half of all cases of bronchiolitis. Other viruses associated with bronchiolitis include rhinovirus (the common cold virus), influenza (flu) , human metapneumovirus, adenovirus , coronavirus, and parainfluenza. Childcare attendance and exposure to cigarette smoke also can increase a child's risk for bronchiolitis.
Although it's often a mild illness, some babies are at risk for severe bronchiolitis — including those who were born prematurely , have a chronic heart or lung disease, or have a weakened immune system due to illness or medicines. Those infants need to be treated in a hospital.
Kids who have had bronchiolitis might be more likely to develop asthma later in life. It's not yet clear whether the illness causes or triggers asthma, or whether kids who eventually develop asthma were just more prone to developing bronchiolitis as infants. Experts continue to study the relationship between bronchiolitis and the later development of asthma.
SIGNS AND SYMPTOMS
The first symptoms of bronchiolitis are usually the same as those of a common cold:
- stuff nose and congestion
- runny nose
- cough
- fever
These symptoms last a day or two and are followed by worsening of the cough and wheezing (high-pitched whistling noises when exhaling).
Sometimes, more severe respiratory difficulties gradually develop. Signs to watch for include:
- fast, shallow breathing
- a rapid heartbeat
- retractions — when the areas below the ribs, between the ribs, and in the neck sink in as a child inhales
- flaring of the nostrils
- irritability, with difficulty sleeping and signs of fatigue (tiredness) or lethargy
- vomiting after coughing
- poor appetite or not feeding well, causing decreased peeing and fewer wet diapers
Sometimes these symptoms can lead to dehydration . Less commonly, babies (especially preemies) may have episodes where they briefly stop breathing (called apnea ) before developing other symptoms.
In severe cases, symptoms may worsen quickly. A child with severe bronchiolitis may get very tired from the work of breathing and have poor air movement in and out of the lungs due to the clogging of the small airways. The skin can turn blue (called cyanosis), which is especially noticeable in the lips and fingernails.
CONTAGIOUSNESS
The infections that cause bronchiolitis are contagious. The germs can spread in tiny drops of fluid from an infected person's nose and mouth, which may become airborne via sneezes, coughs, or laughs, and also can end up on things the person has touched, such as used tissues or toys.
Infants in childcare centers have a higher risk of getting an infection that may lead to bronchiolitis because they're in close contact with lots of other young children.
PREVENTION
The best way to prevent the spread of viruses that can cause bronchiolitis is washing hands well and often. It may help to keep infants away from others who have colds or coughs. Babies who are exposed to cigarette smoke are more likely to develop severe bronchiolitis compared with those from smoke-free homes. So it's important to protect children from secondhand smoke.
There's no bronchiolitis vaccine available yet, but a medication can be given to ease the severity of the disease. It's recommended only for infants at high risk of severe disease, such as those born very prematurely or those with chronic lung or heart disease. The medicine, which contains antibodies to RSV, is given as an injection monthly during peak RSV season.
INCUBATION
The incubation period (the time between infection and the onset of symptoms) ranges from several days to a week, depending on the infection causing the bronchiolitis.
DURATION
Cases of bronchiolitis usually last about 12 days, but kids with severe cases can cough and have wheezing for weeks. The illness generally reaches its peak on the second or third day after coughing begins, causing breathing difficulty before slowly getting better.
PROFESSIONAL TREATMENT
Fortunately, most cases of bronchiolitis are mild and don't need specific professional treatment. Antibiotics aren't useful because bronchiolitis is caused by a viral infection, and antibiotics are only effective against bacterial infections. Medicine may sometimes be given to help open a child's airways.
Infants who have trouble breathing, are dehydrated, or appear fatigued should be checked by a doctor. Those who are moderately or severely ill may need to be hospitalized, watched closely, and given fluids and humidified oxygen. Rarely, in very severe cases, some babies are placed on respirators to help them breathe until they start to get better.
HOME TREATMENT
The best treatment for most kids is time to recover and plenty of fluids. Making sure a child drinks enough fluids can be tricky, though, because infants with bronchiolitis may not feel like drinking. They should be offered fluids in small amounts often.
Indoor air, especially during winter, can dry out airways and make the mucus stickier. Some parents use a cool-mist vaporizer or humidifier in the child's room to help loosen mucus in the airway and relieve cough and congestion. If you use one, clean it daily with household bleach to prevent mold build-up. Avoid hot-water and steam humidifiers, which can be hazardous and can cause scalding.
To clear nasal congestion, try a bulb syringe and saline (saltwater) nose drops. This can be especially helpful just before feeding and sleeping. Sometimes, keeping a child in a slightly upright position may help ease labored breathing.
Acetaminophen can be given to reduce fever and make your child more comfortable. Be sure to give the appropriate dose based on your child's weight.
WHEN TO CALL THE DOCTOR
Call your doctor if your child:
- is breathing quickly, especially if this is accompanied by retractions or wheezing
- might be dehydrated due to vomiting or a poor appetite
- is sleepier than usual
- has a high fever
- has a cough that gets worse
- appears very tired or lethargic
Get immediate help if you feel your child is having difficulty breathing and the cough, retractions, or wheezing are getting worse, or if his or her lips or fingernails appear blue.
Source: Kids Health.org
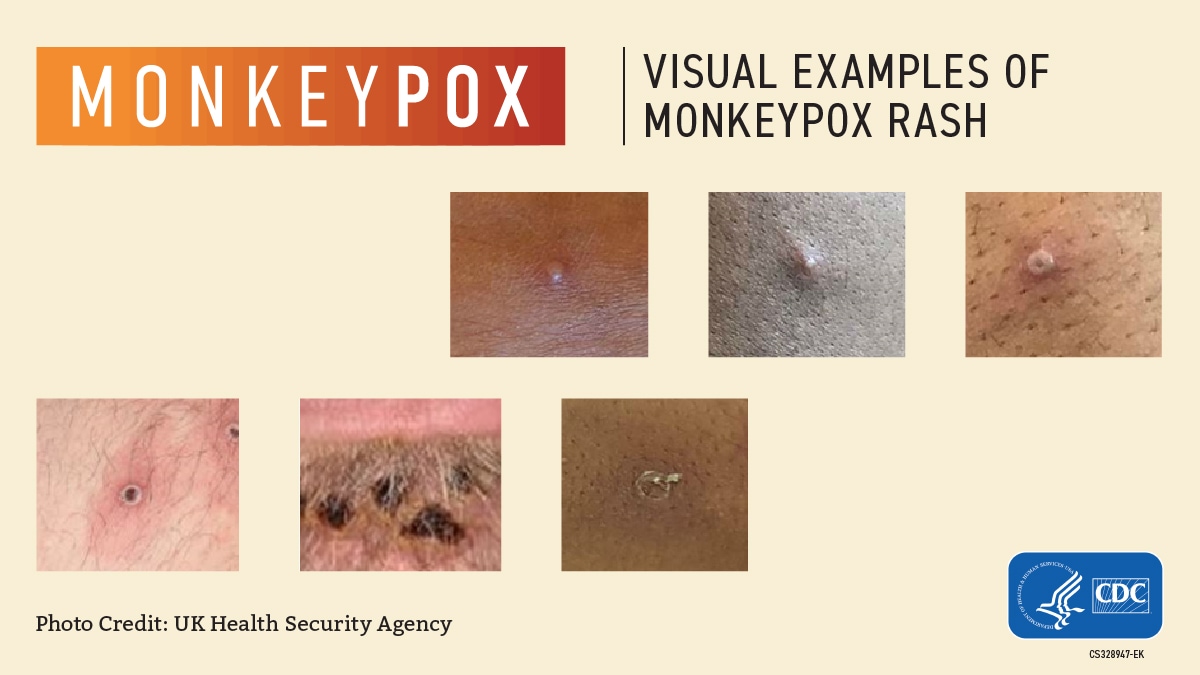
Monkeypox symptoms
People with monkeypox get a rash that may be located on or near the genitals (penis, testicles, labia, and vagina) or anus (butthole) and could be on other areas like the hands, feet, chest, face, or mouth.
The rash will go through several stages, including scabs, before healing.
The rash can initially look like pimples or blisters and may be painful or itchy.
Other symptoms of monkeypox can include:
You may experience all or only a few symptoms
How long do monkeypox symptoms last?
Monkeypox symptoms usually start within 3 weeks of exposure to the virus. If someone has flu-like symptoms, they will usually develop a rash 1-4 days later.
A person with monkeypox can spread it to others from the time symptoms start until the rash has fully healed and a fresh layer of skin has formed. Some people have been found to have infection but no symptoms. To date, however, there is no evidence that monkeypox spreads from people with no symptoms. CDC will continue to monitor for new or changing information about transmission.
If You Have a New or Unexplained Rash or Other Symptoms...
source: cdc.gov
